The movement disorder affects each person differently, but tailoring your treatment for specific symptoms can improve your quality of life.
April 27, 2016
Parkinson's disease, a degenerative disorder of the central nervous system that affects nerve cells in the brain and makes movement difficult, affects an estimated one million people in the United States, according to the National Parkinson Foundation. The disorder is chronic and progressive, affecting the nerve cells that produce dopamine. When these cells become impaired or die, the loss of dopamine leads to abnormal nerve firings and impaired movements, including tremors, loss of balance, and other problems, explains the National Institute of Neurological Disorders and Stroke.
There is no cure yet for the condition, but researchers say they’re piecing together more clues about the roles of genetic and environmental factors. Meanwhile, those diagnosed can take many steps to protect their quality of life and enjoy family, career, and retirement.
If you or a loved one has recently been diagnosed, here are 10 essential facts you need to know:
1. Parkinson's disease is not just an ''old person's
disease." While the disorder is typically
diagnosed at around age 60, younger people can also be affected, says
neurologist and movement disorder specialist Rachel Dolhun,
MD, vice president of medical communications at the The Michael J. Fox Foundation for Parkinson’s
Research. "People who are younger can get this," Dr.
Dolhun says.
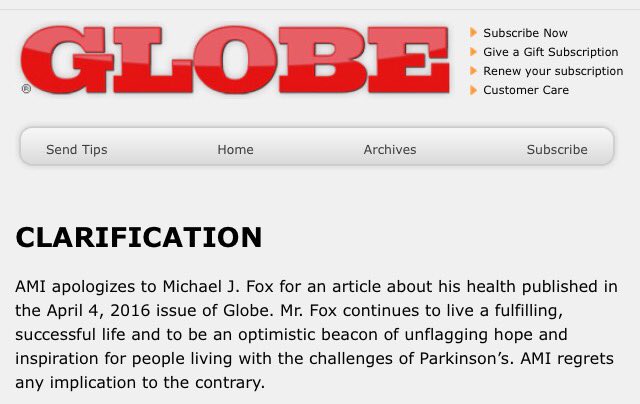
A prominent case in point is actor Michael J. Fox, now 54, who
was diagnosed in 1991 at age 29, she says. "We call it young-onset
Parkinson's at age 40 or under," Dolhun says. More typical, she says, is
to be diagnosed in your 50s or 60s.
2. The cause of Parkinson's is still unknown. A combination of genetic and environmental factors are thought
to contribute to the risk of getting Parkinson's, says Catherine Kopil, PhD,
director of research programs for The Michael J. Fox Foundation. Several
genetic mutations have been found that are linked to Parkinson's disease, and
lifestyle may also play a role. Those who drink caffeine-containing drinks, for
instance, have been found to have a lower risk of getting Parkinson's, although
a cause-and-effect relationship has not been proven.
3. Diagnosing Parkinson's disease isn't simple. There's no specific test to diagnose Parkinson's disease.
Instead, doctors look for four cardinal features of the movement disorder, says
Hubert
Fernandez, MD, the James and Constance Brown Family Endowed Chair in
Movement Disorders and professor of medicine and neurology at the Cleveland
Clinic Lerner College of Medicine in Ohio. His update on Parkinson's disease,
focusing on what is new in diagnostic techniques and treatment, was published
in September 2015 in the Cleveland Clinic
Journal of Medicine.
To diagnose the disease, doctors use the mnemonic TRAP:
• Tremor or shaking at rest, involving
the thumb, entire hand, arm, chin, lips, and feet
• Rigidity felt by the doctor when
rotating a patient's wrist or elbow
• Akinesia or bradykinesia (lack of
movement or slowness of movement) when walking or swinging an arm
• Postural instability, making it
necessary to hold onto something to maintain balance when walking or rising
from a chair
Doctors must rule out other conditions, such as medications that
cause the same symptoms, arthritis, or other medical issues. Observing symptoms,
plus taking a medical history and asking patients if they feel stiff, slow, or
shaky, is how the condition is typically diagnosed.
4. Parkinson's disease isn't just marked by tremors and other
outward symptoms. While those outward symptoms are used
as the basis for a diagnosis, the condition involves much more, Dolhun says.
"There’s a lot that doctors can't see," she says, calling them the
“invisible symptoms” that include sleep problems, constipation, slurred speech,
and mood problems such as depression.
Symptoms vary from one patient to the next, Dolhun says. Indeed,
there's an old saying, "If you’ve met one patient with Parkinson's, you've
met one patient with Parkinson's."
Dr. Fernandez agrees and tells patients that Parkinson's, like
high blood pressure, high cholesterol, and other chronic conditions, needs to
be managed daily. "The more they know, the more they can advocate for
themselves," says Fernandez, who coauthored Ask the Doctor About
Parkinson's Disease with Dr. Okun.
6. Treatment should be tailored to your symptoms and your
preferences. While there is as yet no cure for
Parkinson's disease, treatment can help people live a good quality life. The
primary treatment for the tremors and rigidity is a carbidopa-levodopa combination drug,
like Sinemet and Rytary, which is thought to help replenish the
lost dopamine. But symptoms of Parkinson's disease not only vary from patient
to patient — patients also report that they aren't equally bothered by the same
symptoms, Fernandez says. He always asks his patients: What bothers you most?
For some, he says, it's the constipation.
Others tell him they're bothered by constantly shaking hands (tremor).
"The treatment plan should be tailored to the most pressing
concern," Fernandez says.
7. Clinical trials are worth considering. Every time a Parkinson's disease patient visits their doctor,
Okun suggests they ask, ''What's new? Am I eligible for any new clinical
trial?'' Research is constantly evolving, so it's worth asking if any trials
fit your situation.
"A lot of patients enrolled in clinical trials do better,''
he says, ''partly because they are seen more often." Every clinical trial
has risks and benefits. There is a potential for harm or injury, but the trial
researchers should be sure those risks are minimized in relation to the
benefits. Enrolling may also give access to a treatment not otherwise
available. Before enrollment, trial administrators should spell out the risks
and benefits.
Besides checking in with the doctor, anyone can look up clinical
trials at ClinicalTrials.gov, part
of the National Institutes of Health. The Michael J. Fox Foundation site also
has a trial finder feature that matches
patients with appropriate trials.
8. Stress can make the condition worse; telling people about the
condition can ease it. Stress can increase symptoms,
Dolhun says. For some, one source of that stress is hiding the condition from
coworkers, family, and friends, she says. "The majority of people we talk
to who say they have shared their story with family and friends say they wish
they would have done it sooner," she says.
9. Hospitalizations can be risky. Research has shown that patients with Parkinson's disease are
at risk for getting the wrong medicine at the wrong time, and for contracting infections if
they are hospitalized, which could lead to deterioration in their overall
health. While hospitalization is sometimes necessary, Okun encourages patients
to avoid hospital stays by keeping on top of their treatment plan and taking
medicine as directed — and to get care in an outpatient center or medical
clinic whenever possible.
10. Depression may affect more than half of all patients, and
anxiety affects about 40 percent. Both anxiety and
depression can affect the overall health of someone with Parkinson's even more
than motor symptoms do, according to the National Parkinson Foundation. And
depression and anxiety often occur together, according to research. Fortunately,
treatment helps, and options ranging from exercise to medication and
psychotherapy, or ''talk therapy,'' are plentiful.
By Kathleen Doheny
Reviewed by Samuel Mackenzie, MD, PHD
www.everydayhealth.com/parkinsons-disease/ten-essential-facts-about-parkinsons-disease/