 |
| Sarah Ozinga |
WELCOME TO OUR PARKINSON'S PLACE!
I HAVE PARKINSON'S DISEASES AND THOUGHT IT WOULD BE NICE TO HAVE A PLACE WHERE THE CONTENTS OF UPDATED NEWS IS FOUND IN ONE PLACE. THAT IS WHY I BEGAN THIS BLOG.
I COPY NEWS ARTICLES PERTAINING TO RESEARCH, NEWS AND INFORMATION FOR PARKINSON'S DISEASE, DEMENTIA, THE BRAIN, DEPRESSION AND PARKINSON'S WITH DYSTONIA. I ALSO POST ABOUT FUNDRAISING FOR PARKINSON'S DISEASE AND EVENTS. I TRY TO BE UP-TO-DATE AS POSSIBLE.
I AM NOT RESPONSIBLE FOR IT'S CONTENTS. I AM JUST A COPIER OF INFORMATION SEARCHED ON THE COMPUTER. PLEASE UNDERSTAND THE COPIES ARE JUST THAT, COPIES AND AT TIMES, I AM UNABLE TO ENLARGE THE WORDING OR KEEP IT UNIFORMED AS I WISH. IT IS IMPORTANT TO UNDERSTAND I AM A PERSON WITH PARKINSON'S DISEASE. I HAVE NO MEDICAL EDUCATION,
I JUST WANT TO SHARE WITH YOU WHAT I READ ON THE INTERNET. IT IS UP TO YOU TO DECIDE WHETHER TO READ IT AND TALK IT OVER WITH YOUR DOCTOR. I AM JUST THE COPIER OF DOCUMENTS FROM THE COMPUTER. I DO NOT HAVE PROOF OF FACT OR FICTION OF THE ARTICLE. I ALSO TRY TO PLACE A LINK AT THE BOTTOM OF EACH ARTICLE TO SHOW WHERE I RECEIVED THE INFORMATION SO THAT YOU MAY WANT TO VISIT THEIR SITE.
THIS IS FOR YOU TO READ AND TO ALWAYS KEEP AN OPEN MIND.
PLEASE DISCUSS THIS WITH YOUR DOCTOR, SHOULD YOU HAVE ANY QUESTIONS, OR CONCERNS. NEVER DO ANYTHING WITHOUT TALKING TO YOUR DOCTOR FIRST..
I DO NOT MAKE ANY MONEY FROM THIS WEBSITE. I VOLUNTEER MY TIME TO HELP ALL OF US TO BE INFORMED.
I WILL NOT ACCEPT ANY ADVERTISEMENT OR HEALING POWERS, HEALING FROM HERBS AND ETC. UNLESS IT HAS GONE THROUGH TRIALS AND APPROVED BY FDA. IT WILL GO INTO SPAM.
THIS IS A FREE SITE FOR ALL WITH NO ADVERTISEMENTS
THANK YOU FOR VISITING! TOGETHER WE CAN MAKE A DIFFERENCE!
TRANSLATE
Friday, July 25, 2014
iPads for Balance? PDF Fellow Uses Everyday Technology to Help People with Parkinson’s
Smart Glasses Can Improve Gait of Parkinson’s Patients

Smart Glasses Can Improve Gait of Parkinson’s Patients

Source: University of Twente press release
Image Source: The image is credited to the University of Twente and is adapted from the press release.
Thursday, July 24, 2014
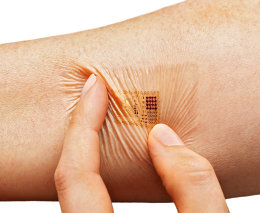
WHEN WEARABLE TECH SAVES YOUR LIFE, YOU WON’T TAKE IT OFF
FAST COMPANY
For Parkinson's Patients, Communications With Doctors Is Life & Death

"The Internet of Healthy Things"
Wednesday, July 23, 2014
Tuesday, July 22, 2014
Why Do I Keep Doing This? Impulsivity

What You Need to Know
The ICDs found in people living with Parkinson’s include:
•Compulsive shopping
•Hypersexuality
•Hoarding
•Compulsive computer usage
“I gambled away more than $450,000 that was supposed to be part of my retirement.” – Walter, diagnosed at age 62
“I bought 110 birdhouses last weekend. I don’t know why. They won’t do me any good. I live in an apartment.” – Carl, diagnosed at age 65
“A friend of mine who was a conservative Christian pastor with a large congregation called me one day. He wanted to let me know that he was leaving the state because he had left his wife of 20 years and their three children. He said he had discovered his ‘soul mate’ at a Parkinson’s support group. She was leaving her husband and two children. He told me that he thought the dopamine agonists that both of them were taking might have had something to do with the situation but that he felt helpless to stop himself. I have not heard from him or any news about him in five years.” – Name withheld by request
What can be done to treat medication-induced impulse control disorders?
•Taper off and stop the drug completely.
•Switch to a different medication.
•Refer you to a psychotherapist who will help you to identify any cues that trigger the urge to gamble or shop, and then identify actions you might take to deal with those urges.
•Connect you with a social worker or social service agency that can refer you to support groups that deal with impulse control disorders.
•Refer you to a psychiatrist who may prescribe naltrexone, a drug that is used to treat alcohol and narcotic abuse. It is generally considered when nothing else has worked.
Monday, July 21, 2014
Parkinson’s Progression Marker Initiative Reports Reduced Tau found in CSF of Parkinson’s subjects
Parkinson’s Progression Marker Initiative Reports Reduced Tau found in CSF of Parkinson’s subjects

